
America was facing mental health challenges prior to the COVID-19 pandemic that were fueled, in part, by an epidemic of loneliness that continues today. Our published studies show that loneliness impacts many people of all ages and all demographic groups across the country, and is particularly problematic among workers. Now, according to new, confirmatory data from Morning Consult commissioned by Cigna, more than half of U.S. adults (58%) are considered lonely. This is fairly consistent with pre-pandemic research that showed 61% of adults experiencing loneliness in 2019, after a seven percentage point increase from 2018.
Loneliness and mental health concerns often go hand-in-hand. The new data shows that adults with mental health issues are more than twice as likely to experience loneliness as those with strong mental health. Given this association and widespread mental health concerns following the pandemic, the need to continue to raise awareness about loneliness remains. It impacts us every day, everywhere, and while society adjusts to the new normal of work, family, social interaction, health and safety, it’s essential that efforts to address loneliness and improve mental wellness continue. This report looks at the state of loneliness among U.S. adults in December 2021 and highlights any notable changes and similarities to Cigna's 2019 and 2018 loneliness research.
Disparate Experiences of Loneliness across Demographics
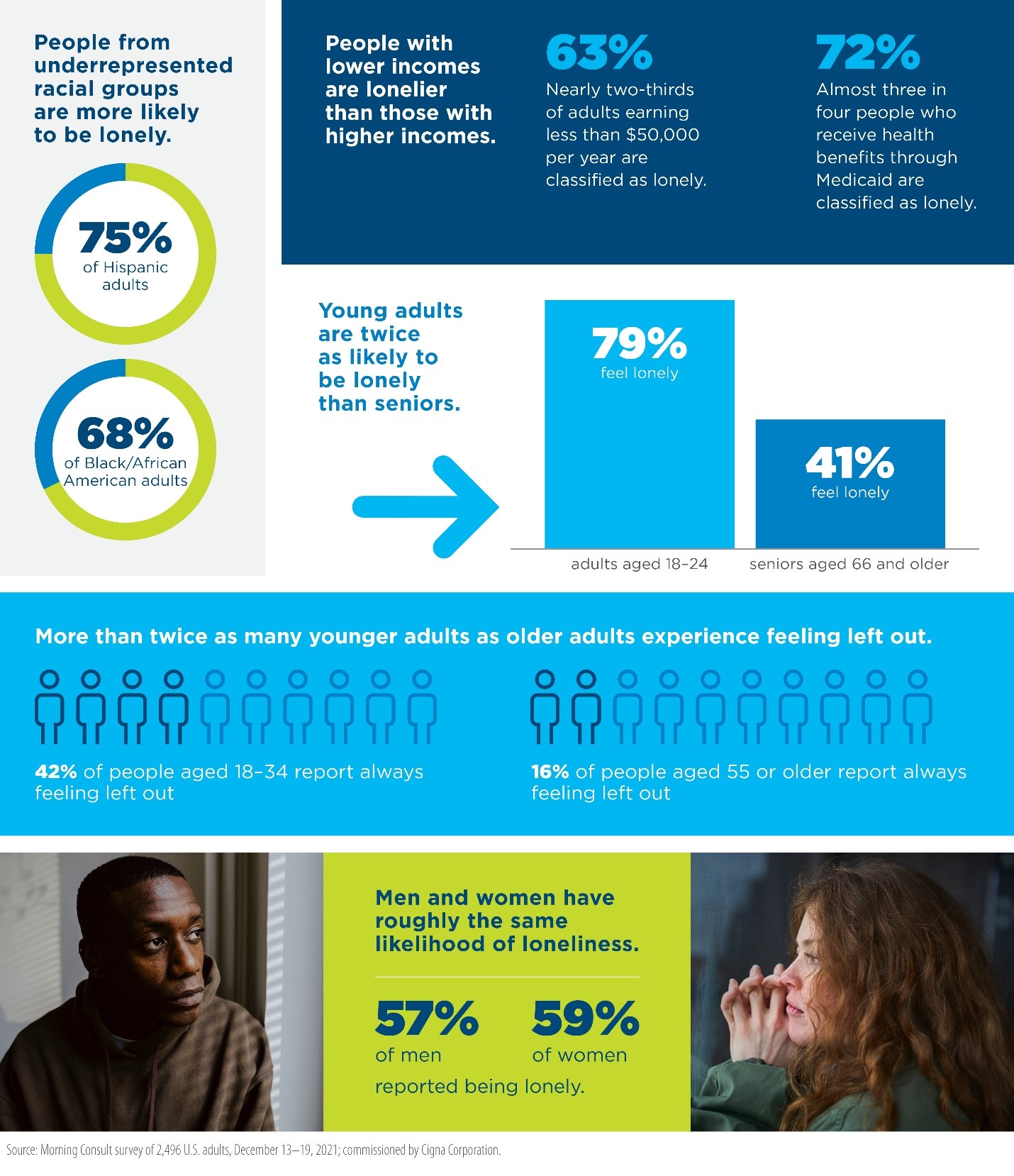
Like most aspects of health and well-being, personal factors including race, age, gender, and income play a role in how individuals and communities experience loneliness — and some people are impacted more than others.
-
People from underrepresented racial groups are more likely to be lonely. 75% of Hispanic adults and 68% of Black/African American adults are classified as lonely – at least 10 points higher than what is seen among the total adult population (58%). This is notably different than previous data which showed similar experiences of loneliness across racial and ethnic groups.
-
People with lower incomes are lonelier than those with higher incomes. Nearly two-thirds of adults (63%) earning less than $50,000 per year are classified as lonely. This is 10 points higher than those earning $50,000 or more. Relatedly, almost three in four people (72%) who receive health benefits through Medicaid are classified as lonely, which is substantially more than the 55% of adults covered by private, employer- or union-provided health insurance benefits.
-
Young adults are twice as likely to be lonely than seniors. 79% of adults aged 18 to 24 report feeling lonely compared to 41% of seniors aged 66 and older. This is consistent with earlier research.
-
More than twice as many younger adults as older adults experience feeling left out. More than two in five adults (42%) aged 18 to 34 report “always” feeling “left out,” compared to just 16% of people aged 55 or older who say the same.
-
Men and women have roughly the same likelihood of loneliness. 57% of men and 59% of women reported being lonely. Loneliness levels were close to equal in 2018 as well, with 53% of men and 54% of women reporting feelings of loneliness. In 2019, data showed a spike in loneliness among men, with 63% experiencing loneliness compared to 58% of women.
Parents and Guardians More Likely to Be Lonely than Non-Parents
During the pandemic, KFF Health Tracking polls found that adults in households with children were more likely to report negative mental health impacts than adults in households without children, and that in general, mothers were more likely than fathers to experience mental health issues. Similarly, this data shows that as we emerge from the pandemic, parents and guardians of children, and in particular mothers and single parents, are more likely to experience feelings of loneliness than those without children.
-
About 65% of parents and guardians are classified as lonely, a 10-point gap compared to non-parents (55%). They also report a strong sense of feeling left out, as 42% of lonely parents always feel this way compared to 24% lonely non-parents.
-
Mothers are especially likely to be considered lonely (69%) – seven points higher than the rate of loneliness among fathers (62%).
-
Single parents are particularly likely to struggle with loneliness, as more than 77% classify as lonely.
Family Connections Impact Feelings of Loneliness
How people feel about their family relationships is a driving force in feelings of loneliness. Adults experiencing loneliness are significantly less likely to discuss their feelings with, or receive support from, their families.
-
Just a third of lonely adults (34%) report talking to their family or partner about how they feel "quite a bit" or "a lot" – half the rate that non-lonely people do (68%).
-
Less than half of lonely adults (45%) report that their family has usually supported them through life either “quite a bit” or “a lot,” compared to 78% of non-lonely adults.
-
When looking closer at the 65% of parents and guardians who are lonely, they may actually have stronger family support than people who are lonely without children. Half of lonely parents reported that, “my family has usually supported me in life” applies “quite a bit” or “a lot” to them, versus 43% of lonely non-parents.
Physical and Mental Health Associated with Loneliness
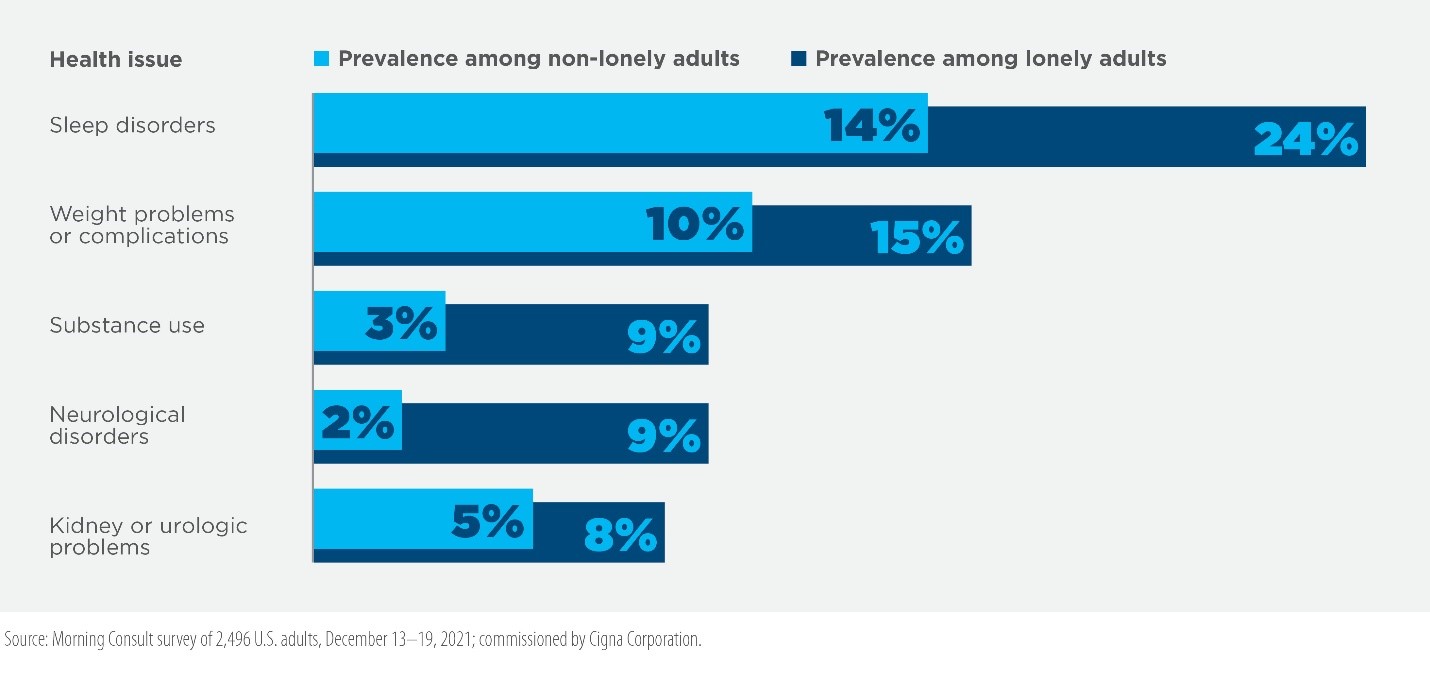
Like the 2019 and 2018 loneliness research, people that report being in fair or poor physical or mental health exhibit more signs of loneliness. This doesn’t mean one causes the other, but there are associations between physical health, mental health, and loneliness that can inform approaches to health and wellness.
-
Adults with physical health issues are approximately 50% more likely to be lonely than those with strong physical health. 77% of adults classified as having fair or poor physical health are experiencing loneliness, while only half (50%) of those with excellent or very good physical health are lonely. In addition, adults classified as lonely are significantly more likely to be diagnosed with or receiving care for a range of health issues including sleep disorders, weight problems, substance use, and others.
- Americans with mental health issues are more than twice as likely to be lonely than those with strong mental health. One in four adults are classified as having fair or poor mental health, and among them, 85% are lonely compared to 42% of adults with excellent or very good mental health. One in three lonely adults (33%) are currently diagnosed with or receiving medical treatment for a behavioral or mental health condition such as anxiety, depression, bi-polar disorder, etc. – more than double the 14% of non-lonely adults diagnosed or receiving treatment for such conditions.
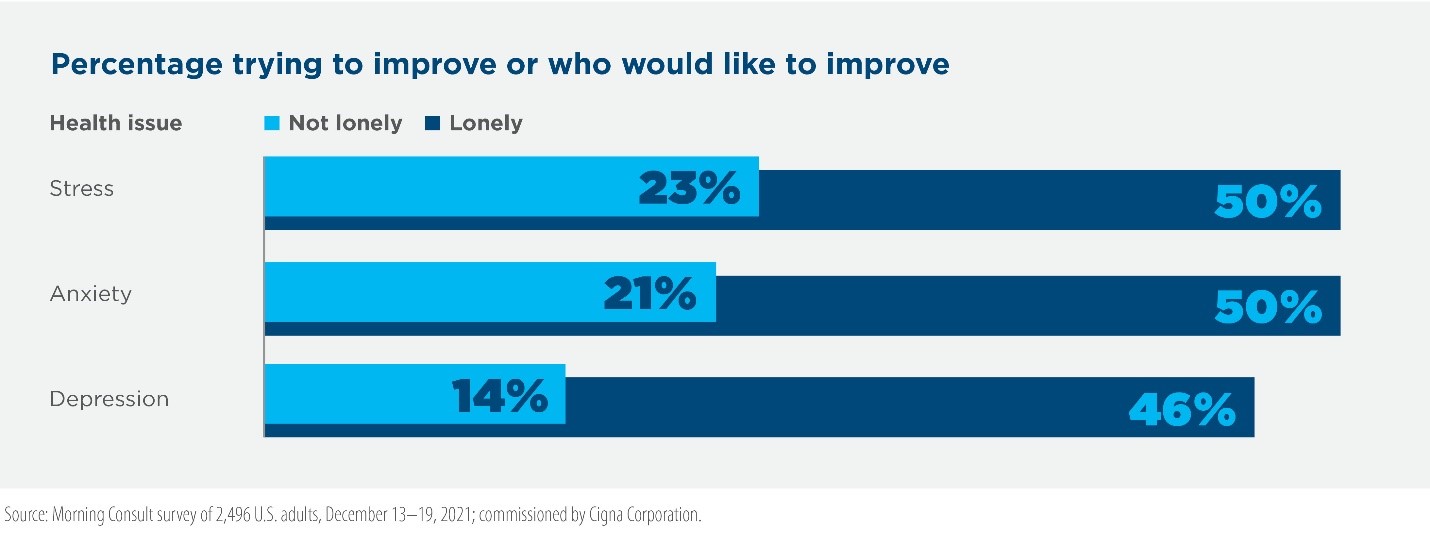
- Loneliness often goes hand-in-hand with other mental health challenges. As stigma and access present barriers to mental health care, responses suggest that even more lonely people struggle with a range of mental health challenges including stress, anxiety and depression, regardless of having a diagnosis or receiving treatment.
Loneliness Impacts People at Work
Loneliness often results in unengaged employees, lower productivity and decreased performance, imposing real costs on businesses – including an estimated $154 billion annually in stress-related absenteeism alone. 2019 data found that lonely employees are more than twice as likely as those who are not lonely to miss a day of work due to illness and more than five times as likely to miss work due to stress. They are also three times more likely to admit they are less productive than most workers with a similar job. New data confirms these trends.
- Loneliness can be a barrier to employee productivity. Less than half of lonely employees say they are able to work efficiently (47%) and perform to the best of their abilities (48%), compared to about two-thirds of non-lonely employees who are able to perform efficiently (64%) and at their peak performance (65%). In addition, more than 42% of lonely employees said they were “mentally somewhere else” while at work in the past three months – more than double that of non-lonely workers (18%).
- Employees experiencing loneliness are more likely to be dissatisfied with their job. Lonely employees are more than three times as likely to be dissatisfied with their job (21%) as employees who are not lonely (7%).
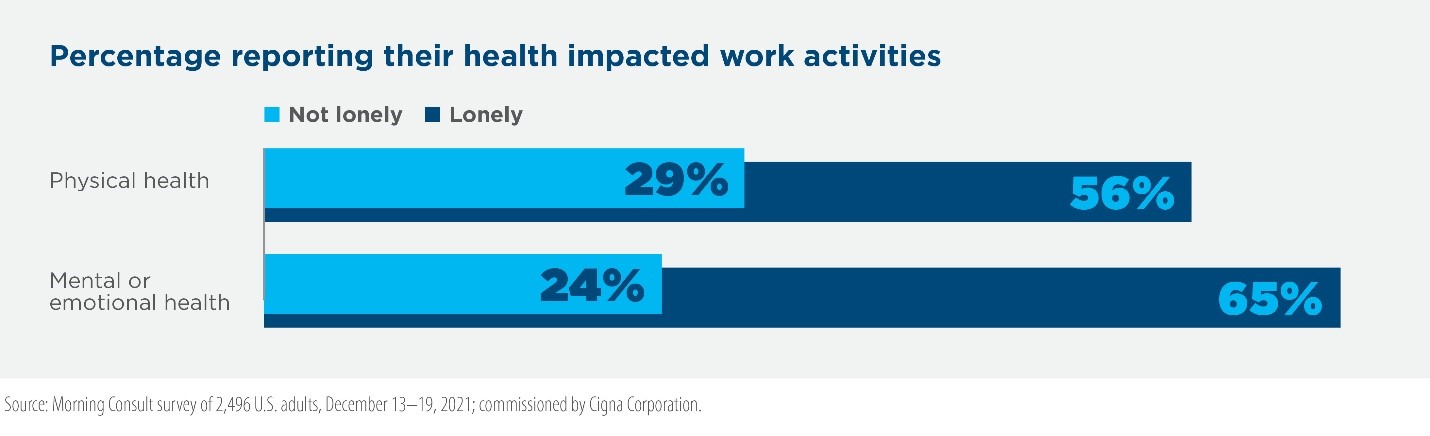
- The poor health associated with loneliness can interfere with workplace performance. Three in 10 employees who are lonely report not feeling well or feeling sick while at work in the past three months, compared to just 14% of non-lonely employees. More lonely employees reported that their physical or mental and emotional health interfered with their normal work-related activities or performance at least moderately in the past four weeks compared to non-lonely workers. Nearly one in five lonely employees (19%) reported that their mental or emotional health “extremely” interfered with work in the last month alone.
Confronting the Loneliness Epidemic
While the loneliness epidemic continues, the fact that loneliness levels mostly remained static despite the pandemic can be viewed as a bright spot – but, not one that doesn’t require action. Young adults, who make up the majority of the future U.S. workforce, are still much more likely to be lonely than older adults. The lack of connectivity with family, friends, and colleagues that in many ways was reinforced during the pandemic remains a key indicator of loneliness. Poor physical and mental health, also reinforced during the pandemic, remain key indicators as well. The fact remains that there is much more work to be done writ large and among specific populations.
For the first time since Cigna began tracking loneliness in 2018, adults who identify with underrepresented racial and ethnic groups are now more likely to be lonely than the total adult population, as well as the total White population – by at least 10 points. While this aligns with the disparate impact the pandemic had on the health and well-being of people from underrepresented groups in this country, it is a new indicator of inequities that should be addressed.
It will take private and public sectors coming together to drive systemic change, but employers can take more immediate steps to help their community of employees build and maintain their health, strength, and energy. They can start by focusing on those who are more likely to be experiencing loneliness – younger people, people from underrepresented groups, and parents – and find new ways to intervene and engage. Three things employers can do today:
- Help build and reinforce social connectivity at work and in the community. Prioritize activities that bring people together in-person and virtually. Leverage all opportunities, including team meetings and events, volunteer activities, employee resource groups, and more to establish connections between coworkers, managers, and senior leaders. Even larger meetings, such as town hall events, can boost connectivity by featuring employees, inspirational customer stories, and real-time engagement opportunities.
- Demonstrate flexibility, and offer health and well-being benefits that meet current and evolving needs. Reinforce the importance of mental health by prioritizing work-life balance and encouraging the use of paid time off. Provide a spectrum of services and support for mental health concerns impacting employees and their families, and work to destigmatize utilization.
- Bring the importance of diversity, equity, and inclusion to life. Build and reinforce an environment that is open to meaningful dialogue and understanding, an environment that is safe and welcoming for everyone, and an environment that is fair and equitable. People want to feel purpose and they want to feel they belong.
About this report: Commissioned by Cigna Corporation, Morning Consult conducted a survey of 2,496 U.S. adults from December 13-19, 2021. Results have an unweighted margin of error of ±2 percentage points. Comparisons are made to the 2020 Cigna Loneliness Index survey data from an Ipsos survey of 10,400 U.S. adults in July 2019. Comparisons are also made to the 2018 Cigna Loneliness Index survey data from an Ipsos survey of 19,000 U.S. adults in February 2018.

The Business Case for Addressing Loneliness in the Workforce
There are five key workforce factors that employers can support in order to reduce employee loneliness within their organizations, as well as promote employee engagement and psychosocial health.